CASE DISCUSSIONS
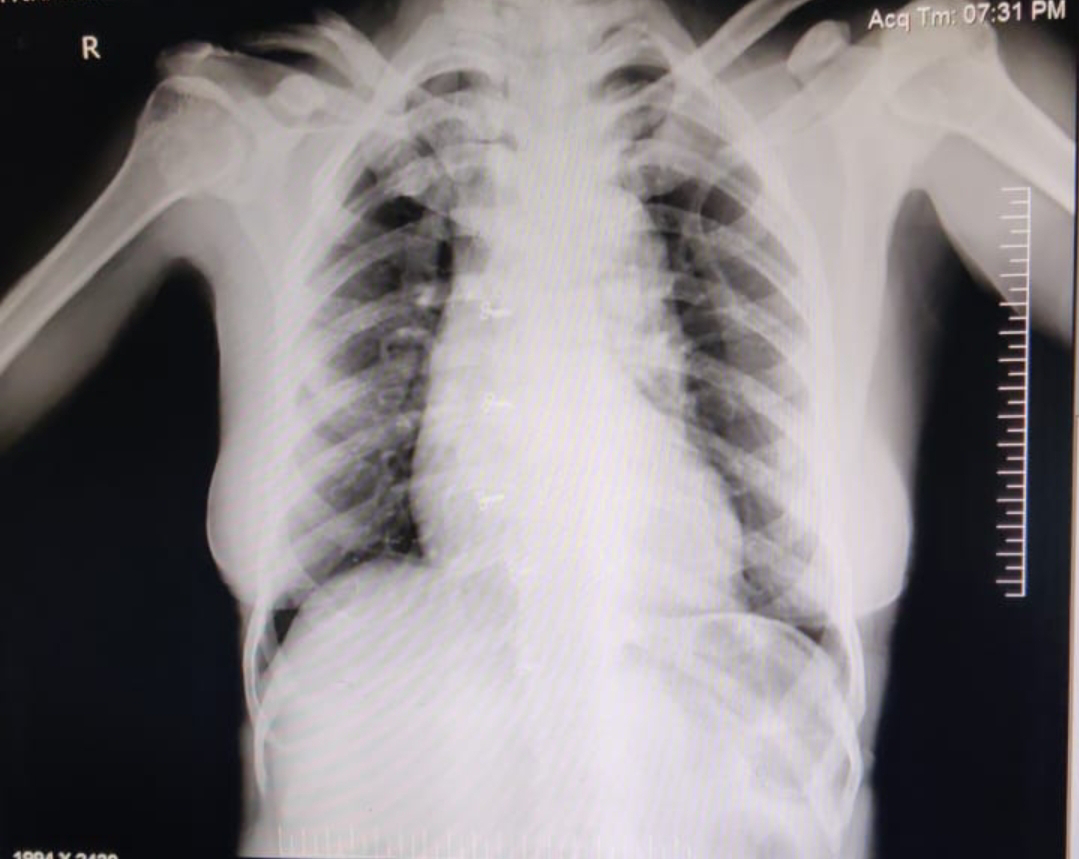
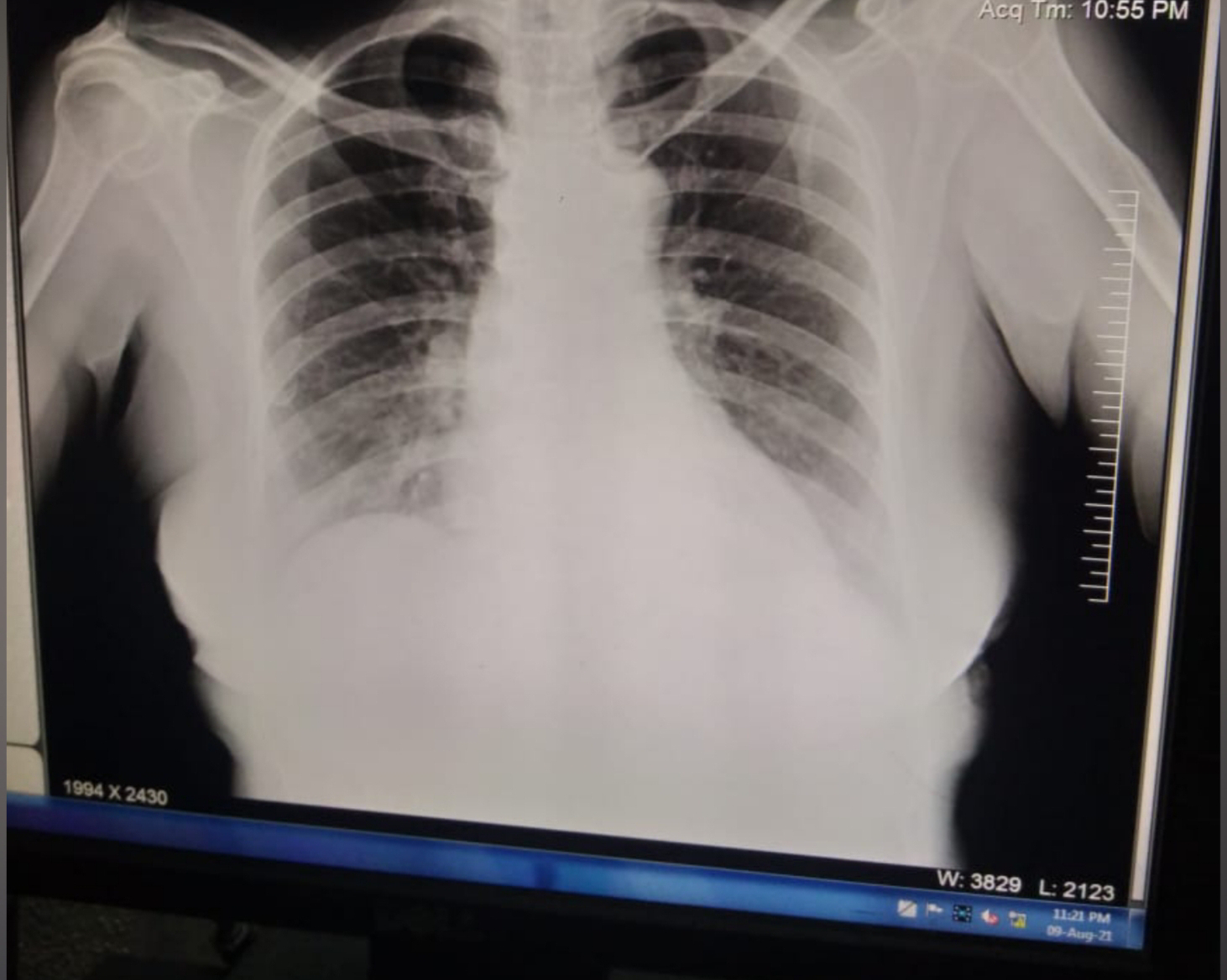
45YR old male, real-estate business man, came to OPD with cheif complaints of 1.VOMITINGS , 2-3 episodes per day since 1week. 2. HEMETEMESIS , 2episodes , 10-15ml , 1week back. 3. MELENA since 2days. No H/O fever, pain abdomen, diarrhoea. Not a K/C/O DM, ASTHMA,TB. PAST HISTORY: 2yrs back, when he was at home around 11-12pm , he had INVOLUNTARY MOVEMENTS OF LEFT UL,LL DROOLING+ DEVIATION OF MOUTH+ ROLLING OF EYE BALLS + then he fell down. INVOLUNTARY MOVEMENTS LASTED FOR ABOUT 5MIN. He was in POST ICTERAL CONFUSION STATE FOR ABOUT HALF HOUR. Then he was taken to hospital, where his BP WAS HIGH. started on ANTI HYPERTENSIVES and ANTI EPILEPTICS. ANTI HYPERTENSIVE - NOT DOCUMENTED. ANTI EPILEPTICS: LEVIPIL 500MG /BD He continued to use these medications for almost one and half yr , and stopped using anti epileptic medication 1mon back. Now these acute complaints since 1week. LAST BINGE OF ALCOHOL 3DAYS BACK. no sign...