General medicine case
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
CHIEF COMPLAINTS:
A 70 year old female patient resident of Aliya who stays at home came to the OPD with chief complaints of:
- Fever since 1 week
-Right buttock pain since 3 days
-H/o loose stools and vomiting 5 days ago which were subsided.
HISTORY OF PRESENT ILLNESS:
- patient was apparently asymptomatic 2 years ago then due to loss of appetite and generalized weakness patient visited local Hospital and was diagnosed with type 2 diabetes milletus. Since then she was on Oral hyperglycemic agents (unknown).
- 2 months ego patient experienced 1 episode of sudden onset of giddiness and generalized weakness which reduced in 30 minutes on giving IV fluids.
- she was shifted to TAB. Metformin 500 mg PO/OD
- patient complaints of fever since one week ,high grade ,intermittent with subsided on medication. No chills and Rigor.
- History of three episodes of vomiting nonbilious,non projectile ,non blood tinged containing food particles for one day.
- History of 3-4 episodes of loose stools, watery for one day which subsided on its own.
- patient visited OPD and was prescribed antibiotics but her fever did not subside and complained of generalized weakness, loss of appetite and lack of sleep.
- History of right buttock pain since 3 days no history of trauma or any injections taken outside. Pricking type of pain radiating to thighs.
- No history of decreased urine output, shortness of breath ,chest pain ,pedal edema, cough.
PAST HISTORY :
-No history of HTN, CAD, asthma, tuberculosis.
-know case of DM since 2 yrs.
PERSONAL HISTORY :
-loss of appetite
-bowel and bladder-regular
-no addictions
FAMILY HISTORY :
-No significant family history.
GENERAL EXAMINATION :
patient is conscious, coherent, co-operative.
Temp-afebrile
PR-91 bpm
BP-100/70 mm of Hg
RR-20/min
Spo2-98% at room air
Pallor-present
No icterus, cyanosis,clubbing, lymohadenopathy,edema.
CVS:
S1,S2 heard
No murmurs
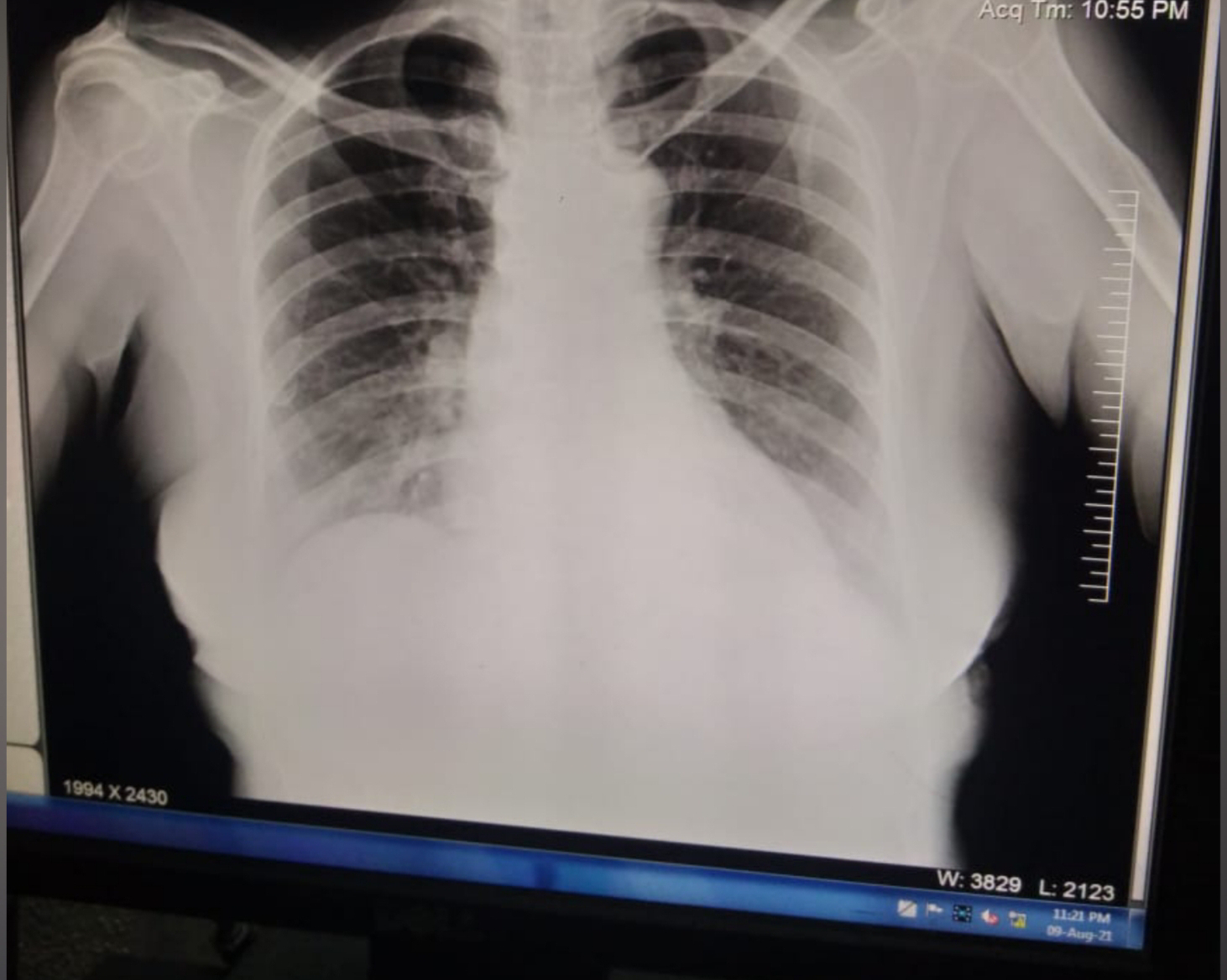
RESPIRATORY SYSTEM :
Bilateral vesicular breath sounds heard
Treachea central
No added sounds
ABDOMEN:
Shape of abdomen -obese
No tenderness, palpable mass, Hernial orifices,free fluid.
Liver and spleen not palpable
Bowel sounds heard.
CNS:
Level of consciousness - Alert
Speech-normal
No signs of meningeal irritation.
Cranial nerves, motor system, sensory system -normal
Reflexes - present
INVESTIGATIONS:
Hb-8.5
Tlc-14,200
Plt-1.5
S. Urea-103
S. Creatinine -3.1
Sodium-131
Potassium -3.5
Chloride-99
9-8-21
Hb-7.7
Tlc-21,800
Plt-3.49
S. Urea-51
S.creatinine-2.4
Sodium-138
Potassium -3.9
Chloride-100
PROVISIONAL DIAGNOSIS :
PRE-RENAL ACUTE KIDNEY INJURY SECONDARY TO ACUTE GE
PLAN OF TREATMENT :
DAY 1
1.IVF-NS,RL@100 ml /hr
2.INJ.CEFTRIAXONE 1GM/IV/BD
3.INJ.PAN 40MG IV/OD
4.INJ.ZOFER 4MG IV/SOS
5.INJ.H.MIXTARD SC/BD
6.INJ.OPTINEURON 1 AMP in 100 ml NS/IV/OD
7.BP/PR/RR/TEMP CHARTING
8.STRICT I/O CHARTING
DAY 2
1.IVF-NS,RL@100 ml /hr
2.INJ.CEFTRIAXONE 1GM/IV/BD
3.INJ.PAN 40MG IV/OD
4.INJ.ZOFER 4MG IV/SOS
5.INJ.H.MIXTARD SC/BD
6.INJ.OPTINEURON 1 AMP in 100 ml NS/IV/OD
7.BP/PR/RR/TEMP CHARTING
8.STRICT I/O CHARTING
DAY 3
1.IVF-NS,RL@100 ml /hr
2.INJ.CEFTRIAXONE 1GM/IV/BD
3.INJ.PAN 40MG IV/OD
4.INJ.ZOFER 4MG IV/SOS
5.INJ.H.MIXTARD SC/BD
6.INJ.OPTINEURON 1 AMP in 100 ml NS/IV/OD
7.TAB.ULTRACET PO/QID/1/2 TAB
8.CHLORHEXIDINE MOUTH WASH/BD
9.TAB.PCM 650 MG PO/BD
10.BP/PR/RR/TEMP CHARTING
11.STRICT I/O CHARTING.




Comments
Post a Comment